Abstract
T-cell Replete HLA-haploidenitcal donor transplantation (HIDT) with post-transplant cyclophosphamide is increasingly considered an acceptable alternative for patients lacking timely access to an optimally matched related (MRDT) or unrelated donor (MUDT). Multiple recent registry and single center studies have shown comparable overall survival and disease free survival rates among the three donor sources with a significantly lower risks of acute and chronic GVHD among HIDT recipients(1). Donor age may also affect outcomes. Many candidates for allogeneic HCT will have access to multiple available donor sources. In this situation, it is unclear whether outcomes can be improved using a younger HID rather than an older MRD or MUD.
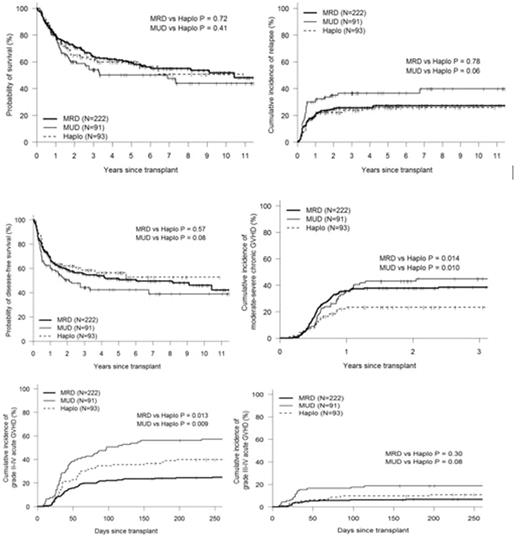
We analyzed 406 consecutive allogenic HCT recipients, median age of 54 years (range 19, 77) comparing outcomes after a MRDT (n-222) or MUDT (n-91) using a donor ≥ 35 years old to HIDT performed using donors aged ≤ 35 years (n=93). Survival was calculated using the Kaplan-Meier estimator. Univariate analysis with Gray test and log-rank test were used for cumulative incidence and survival respectively. Pointwise comparison at 3 years post HCT was performed using the Wald test. Median follow up for survivors was 51.5 months. Compared to MRDT and MUDT, HIDT recipients had similar median age at time of HCT, hematopoietic cell transplant comorbidity index (HCT-CI), disease risk index (DRI) distribution and donor recipient sex matching. Recipients of HIDT were more likely to have received TBI based Myeloablative conditioning (39% vs 18% and 11% for MUDT and MRDT, p <0.001), bone marrow graft source (33% vs 11% and 2% for MUDT and MRDT, p<0.001) and more likely to be transplanted after 2011 (79% vs 56% and 56% for MUDT and MRDT, p<0.001). The median donor age for HIDT of 27 years (range 15, 34) was significantly younger than MRDT 53 years (range 35, 77) and MUDT 41 (35, 64), p=0.001. The survival estimates and relapse incidence at 1 and 3 years respectively post HCT were: OS (80% and 64% for MRDT, 79 and 54% for MUDT, 79% and 62% for HIDT), DFS (69% and 55% for MRDT, 61% and 44% for MUDT, 66% and 58% for HIDT), TRM (11% and 19% for MRDT, 8% and 16% for MUDT, 12% and 18% for HIDT), and relapse (20% and 26 % for MRDT, 31% and 37% for MUDT, 22% and 24% for HIDT). HIDT recipients had better 3-year relapse rates (p=0.048) and DFS (p=0.042) compared to MUDT with similar overall survival. Recipients of HIDT also had significantly lower incidence of moderate-severe chronic GVHD compared to MRDT and MUDT (23% HIDT vs 45% for MUDT and 38% for MRDT, p=0.01). When limiting the analysis to recipients age ≥ 50 years (n=258), there was no difference in OS, DFS or relapse between the 3 donor sources.
Recipients of HIDT from a young donor ≤35 years, have similar overall survival and lower rates of chronic GVHD compared to transplants using MRD or MUD donor ≥ 35 years. Moreover, HIDT recipients have lower relapse and better DFS compared to MUDT. This study suggests that given a situation where a choice between a young Haploidenitcal relative and an older matched unrelated donor is to be made, one can achieve better disease free survival with haploidentical donor and significantly lower rates of chronic GVHD.
1. Ciurea SO, Zhang MJ, Bacigalupo AA, Bashey A, Appelbaum FR, Aljitawi OS, et al. Haploidentical transplant with posttransplant cyclophosphamide vs matched unrelated donor transplant for acute myeloid leukemia. Blood. 2015;126(8):1033-40.
Figure 1: Kaplan-Meier and Cumulative Incidence Curves for OS, DFS, Relapse, cGVHD, Grade II-IV and III-IV acute GVHD
Solh: ADC Therapeutics: Research Funding; Celgene: Speakers Bureau; Amgen: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal